Tardive dyskinesia assessment and diagnosis
Make screening a part of your routine for all patients on antipsychotics
2020 American Psychiatric Association guidelines recommend1:
-
1
Screening for TD before starting or changing patients’ dopamine receptor blocking agent (DRBA) treatment
-
2
Monitoring for signs of TD at each visit
-
3
Conducting a structured TD assessment every 6 to 12 months, depending on patient’s risk, and if new or worsening movements are detected at any visit
The involuntary and uncontrollable movements from TD may
not only impact your patients physically, but also emotionally2
When assessing the signs of tardive dyskinesia, ask about how it is affecting their everyday lives.
ASK ABOUT TD IMPACT
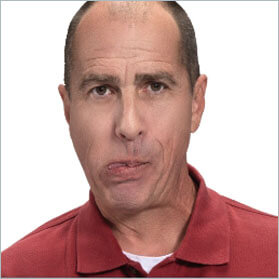
Tardive dyskinesia (TD) doesn’t just present in the face and mouth—involuntary movements may impact upper and lower limbs, the neck, and trunk3,4
UPPER LIMBS

Asymmetrical movements, swaying, “piano fingers,” grabbing of clothing3,4
LOWER LIMBS

Splayed or hyperextended toes, gripping, ankle twisting3,4
TORSO
Hyperextension, shifting, rocking3,4
TONGUE
“Bonbon” sign, protrusion, darting3,4
EYES

Excessive blinking and squinting3,4
LIPS
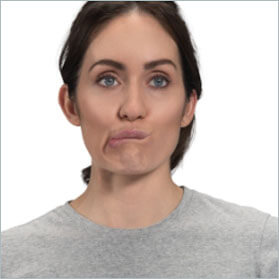
Smacking, puckering, pursing3,4
JAW

Biting, clenching, lateral movements, chewing3,4
Actor portrayals
Take the TD Challenge: Assessment and diagnosis
Can you differentiate tardive dyskinesia from drug-induced parkinsonism and other acute drug-induced movement disorders?
Put your knowledge to the test.
EXPERT PERSPECTIVES:
Tardive dyskinesia (TD) is clinically distinct
Dr. Laxman Bahroo, from Georgetown University’s Neurology Department, discusses the clinical distinctions between TD and acute drug-induced movement disorders and what to look for.
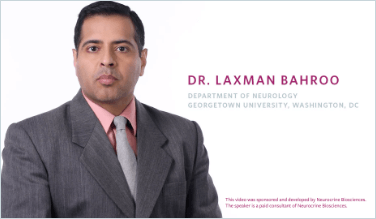
EXPERT PERSPECTIVES:
Tardive dyskinesia (TD) is clinically distinct
Dr. Laxman Bahroo, from Georgetown University’s Neurology Department, discusses the clinical distinctions between TD and acute drug-induced movement disorders and what to look for.
REFERENCES:
- Keepers GA, Fochtmann LJ, Anzia JM, et al. The American Psychiatric Association Practice Guideline for the Treatment of Patients With Schizophrenia. 3rd ed. American Psychiatric Association Publishing, 2020.
- McEvoy J, Gandhi SK, Rizio AA, et al. Effect of tardive dyskinesia on quality of life in patients with bipolar disorder, major depressive disorder, and schizophrenia. Qual Life Res. 2019;28(12):3303-3312.
- Guy W. ECDEU Assessment Manual for Psychopharmacology. Revised 1976. Rockville, MD: National Institute of Mental Health; 1976.
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Arlington, VA: American Psychiatric Association; 2013.
- Task Force on Tardive Dyskinesia. Tardive Dyskinesia: A Task Force Report of the American Psychiatric Association. Washington, DC: American Psychiatric Association; 1992.
- Bhidayasiri R, Jitkritsadakul O, Friedman JH, Fahn S. Updating the recommendations for treatment of tardive syndromes: a systematic review of new evidence and practical treatment algorithm. J Neurol Sci. 2018;389:67-75.
- Caroff SN, Citrome L, Meyer J, et al. A modified Delphi consensus study of the screening, diagnosis, and treatment of tardive dyskinesia. J Clin Psychiatry. 2020;81(2):19cs12983.
REVIEW EFFICACY IN TD
Explore how INGREZZA® (valbenazine) capsules reduced TD severity in both short- and long-term studies of adult patients with TD
VISIT EFFICACY IN TDTREAT FIRST LINE WITH VMAT2 INHIBITORS
VMAT2 inhibitors, like INGREZZA, are recommended as first-line treatment for TD1,6,7
VISIT TD GUIDELINESSEE REAL-WORLD RESULTS
WITH INGREZZA
View videos of real-world patients with TD treated with INGREZZA
WATCH CASE VIDEOSREFERENCES:
- Keepers GA, Fochtmann LJ, Anzia JM, et al. The American Psychiatric Association Practice Guideline for the Treatment of Patients With Schizophrenia. 3rd ed. American Psychiatric Association Publishing, 2020.
- McEvoy J, Gandhi SK, Rizio AA, et al. Effect of tardive dyskinesia on quality of life in patients with bipolar disorder, major depressive disorder, and schizophrenia. Qual Life Res. 2019;28(12):3303-3312.
- Guy W. ECDEU Assessment Manual for Psychopharmacology. Revised 1976. Rockville, MD: National Institute of Mental Health; 1976.
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Arlington, VA: American Psychiatric Association; 2013.
- Task Force on Tardive Dyskinesia. Tardive Dyskinesia: A Task Force Report of the American Psychiatric Association. Washington, DC: American Psychiatric Association; 1992.
- Bhidayasiri R, Jitkritsadakul O, Friedman JH, Fahn S. Updating the recommendations for treatment of tardive syndromes: a systematic review of new evidence and practical treatment algorithm. J Neurol Sci. 2018;389:67-75.
- Caroff SN, Citrome L, Meyer J, et al. A modified Delphi consensus study of the screening, diagnosis, and treatment of tardive dyskinesia. J Clin Psychiatry. 2020;81(2):19cs12983.
